PODCAST TRANSCRIPT
Narrator: At the intersection of science and clinical experience in IBD, this is Gut Reactions. Settle in, as our host, Dr. David Rubin, brings leading gastroenterologists together for one-on-one conversations. This podcast is brought to you by AbbVie.
Dr. David Rubin: Welcome to the Gut Reactions Podcast. I'm your host, Dr. David Rubin, Chief of the Section of Gastroenterology, Hepatology, and Nutrition at the University of Chicago, where I'm also the Director of our Inflammatory Bowel Disease Center.
I'm delighted to be joined today by Dr. Joshua M. Steinberg, who is a board-certified gastroenterologist and director of IBD at Gastroenterology of the Rockies, a large GI practice serving patients in Denver and the Boulder, Colorado metropolitan areas. He's also part of the SCL Intermountain Healthcare Network. Wow, that's a mouthful, Josh.
But more importantly, he's an adjunct clinical instructor at the University of Colorado School of Medicine. And Josh and I, out of full disclosure, worked together because he did an advanced fellowship year in IBD at the University of Chicago after he did his regular fellowship at Georgetown. So hi, Josh. How are you doing? Welcome to Gut Reactions.
Dr. Josh Steinberg: Hi David, thanks so much for having me. I'm excited to be here.
Dr. David Rubin: All right, well, we're gonna make sure that you haven't forgotten what we taught you here. So that's part of this. That's the secondary agenda to our podcast today.
Dr. Josh Steinberg: A little pop quiz.
Dr. David Rubin: That'll come later.
Anyway, in our last episode, we talked a lot about treatment targets, and I had a wonderful conversation with Dr. Oriana Damas. But today we're gonna continue the discussion by exploring next steps when patients are not meeting their treatment goals.
Dr. David Rubin: Many moderate to severe patients with UC may not adequately respond to an anti-TNF or other treatments, as we all know, and loss of response can present either as primary or secondary loss of response to that anti-TNF. Just as a reminder to our colleagues, primary loss of response occurs when a patient isn't experiencing an adequate response after starting the therapy. In this case, we're talking about anti-TNFs, and this is usually noticed within the initial weeks or months of starting that therapy. Secondary loss of response, or what I call secondary non-response, occurs when a patient initially responds well to the anti-TNF. They may even experience complete remission, but over time, they have either attenuation, where they're losing response, but still having some response when they get their dose, or complete loss of response. And that can happen within months after starting treatment to years later. So, Josh, tell us a little bit about how you define disease control before we get into sort of the non-responder. Just talk to us about what do you think about when you're starting a patient on therapy to know that it's working, and how do you explain that to your patients?
Dr. Josh Steinberg: It's an important question, David. Disease control is all about addressing the inflammation associated with ulcerative colitis to ensure the symptoms as well as the endoscopic response remain managed. So, in my practice, achieving disease control and a satisfactory treatment response goes well beyond symptom relief. It's about reaching and maintaining clinical remission where symptoms like bleeding are significantly reduced, but we also want to see a reduction in Mayo endoscopic subscores. So steroid-free remission, of course, it is also an important disease control target for patients with UC, since it helps prevent the long-term complications associated with steroid use, but also provides an alternative treatment strategy for those who cannot tolerate steroids. To ensure the authenticity of these improvements, we closely monitor biomarkers. We look at blood tests like CRP, C-reactive protein, as well as fecal calprotectin, and of course we utilize endoscopic measures.
This comprehensive approach to effectively manage the underlying inflammation can lead to better symptom control.
Dr. David Rubin: And that, of course, is very similar to what I do, not surprisingly. And I would also just say that for the patient, I make sure they understand that our goal is remission and that our goal is for them to be stable in remission and to do well. It's interesting because it often comes up when a patient says, am I going to be on this the rest of my life? And I always say, well, let's first make sure the therapy is working.
And then secondly, let's make sure it works as long as we need it until we have something better. And I think it's safe and fair to bring that up and to say that to patients. So, Josh, for patients who demonstrate an initial response to therapy, let's say they're doing okay, what do you do in terms of your ongoing monitoring of these patients to know that they're continuing to respond? What do you choose and how often do you do it?
Dr. Josh Steinberg: So, typically I advise a monitoring schedule that involves regular check-ins. I want to see my patients frequently, especially in the beginning. We're going to schedule visits more frequently every three to six months, if not sooner, to closely track the progress and ensure that response to the therapy is sustained.
Dr. David Rubin: And you mentioned calprotectin already, but do you incorporate that?
Dr. Josh Steinberg: Yeah, calprotectin of course, a noninvasive surrogate marker for inflammation. We're going to use that more frequently. Obviously, this is not as invasive as a colonoscopy. It would be tough sell for our patients to do a colonoscopy every three, four or six months. So, I use that in conjunction with the endoscopic response.
Dr. David Rubin: Yeah, I completely agree. It needs to be benchmarked. And we also, of course, have to remember that sometimes patients don't even want to handle their stool, which is one of the limitations of that test. And there are reasons that it can be falsely positive as well as falsely negative, although that's less common in colitis.
So, Josh, in your experience, what are some of the ways that inadequate responders present to you in clinical practice?
Dr. Josh Steinberg: Yeah, so inadequate responders in clinical practice present in many ways. So, one common scenario is when patients are presenting with breakthrough symptoms, despite their treatments. So, diarrhea, increased stool frequency, rectal bleeding, abdominal pain, rectal urgency. All these symptoms can persist or even worsen as the current therapy is unable to control their inflammation causing these symptoms. Additionally, if a patient finds it difficult to taper off of steroids without their symptoms firing up again, that's really another indication that the disease is not well controlled. Steroids of course are a useful tool, but we don't want to rely on steroids for an extended period of time. Another situation is when patients have symptoms that improve with treatment initially, but when we look at the objective measures, including biomarkers like calprotectin or CRP, we find that there's still underlying inflammation that needs to be addressed. And this tells me that the drug is losing its efficacy and the patient might be at risk for flaring and further ulcerative colitis complications.
Dr. David Rubin: So, Josh, this is obviously a very important conversation, in part because we now have so many different treatment options in ulcerative colitis, and we would like to know when to use them. We also need to know when one therapy isn't working and when to make these decisions. And I'm really glad that you brought up the steroid issue. A patient who's responding to steroids, but when they drop below a certain dose, they have immediate return of their symptoms, or when they've been off steroids for some period of time, they have a relapse and need the steroids again—because this is clearly an indication that the steroid-sparing maintenance therapy is not doing its job. And we have to keep that in mind as an important marker of non-response among all the other things that you nicely identified.
Dr. David Rubin: And we also need to communicate to patients that if they're having breakthrough, if they're not in stable, controlled remission, we need to know about it and we need to think carefully about what we're going to do. So, as you've seen when you worked with me, I routinely ask patients, “Do you have any breakthrough symptoms in anticipation of the next dose of your medicine?” And that's when they tell us about whether they're really doing as well as we hope.
So, Josh, why don't we talk a little bit about the common symptoms that give us a clue that patients may be losing response. When we ask them about how they're doing, what do we hear from them that tells us we should be assessing this more carefully?
Dr. Josh Steinberg: Absolutely. I would say bloody stool is probably the most common symptom and my top reason for concern, followed by diarrhea or increased stool frequency. So, patients may miss or not report rectal bleeding to us directly, since it's not maybe as impactful to them as stool frequency, but blood in the stool could really indicate ongoing inflammation that's not being adequately controlled. When the disease is not controlled, patients can experience a range of symptoms, including weight loss, loss of appetite, and all these symptoms can really seriously impact a patient's day-to-day activities, whether it's their hobbies, their work schedule, parenting duties, and the like. So that’s a really important aspect that we want to take control of when we are starting patients on therapy for their ulcerative colitis.
Dr. David Rubin: So, Josh, do you have any hobbies?
Dr. Josh Steinberg: No hobbies, just work. I'm just kidding. I am a father of two. I like to go out with my kids. We spend a lot of time outside in Colorado where I'm at currently. And yeah, my free time, I love to travel when I get the chance.
Dr. David Rubin: There you go. And, you know, obviously traveling with ulcerative colitis is a big problem if the disease is active. People can't plan a long trip, they can't be in a car without knowing where the next restroom stop might be, and certainly being on a plane. Certainly, if you're in a middle seat or a window seat, you can imagine how someone with uncontrolled colitis can feel and how nervous they are about those types of experiences. So, it does really, truly affect quality of life in major ways.
So, let's talk a little bit about patient's hesitancy to openly discuss all their symptoms during a maintenance appointment. And that can lead to misunderstanding or later loss of control to the point where they get much sicker. So what questions are you asking to try to bring this out when you're talking to the patients?
Dr. Josh Steinberg: So typically, many patients who are in an active flare, they will be direct about sharing their symptoms, but many are not. So, I'll ask the typical common symptom questions, “rectal bleeding, how many stools per day? Are you having urgency? Are you waking up at night to have a bowel movement?” But I'll also ask other questions to really understand how they're functioning in their daily life to understand their disease burden specifically. So, for example, “Are you doing what you want and need to be doing in your daily life? Are you going to work? Are you able to,” if you're a, you know, 20-year-old college student, “make it to class?” If you're a 45-year-old mother of two, “Are you able to take your kids to school and spend time with your family?” Many patients will not be forthcoming in some of their symptoms and how it's really affecting them.
And of course, all of the symptoms and disability that might come with ulcerative colitis can seriously affect a patient's mental and psychosocial health. So, all these things we want to consider and address during a clinic visit.
Dr. David Rubin: I heard someone once say that what they ask patients is, “What are they unable to do because of their current state of their colitis?” And I think that that's a good open-ended question that gets at some of this as well. And because often the patient is compensating for many different ways of their daily existence and avoiding certain behaviors or have changed where they work or how they get to work in the morning or what they're able to do to take care of their kids. And I think that can be a really helpful way to do this.
Dr. David Rubin: And as you know, from working with me, the five questions I always ask patients with colitis is, “Are you having formed stool? Are you sleeping through the night without bowel movements? Do you see blood in your stool? Do you have urgency?” And, “Are you able to pass gas without fear of leaking?” And when a patient is unable to answer those questions properly, we know that they're probably not in symptomatic remission. I also then emphasize to them, even though they're feeling better in some cases, it might not be enough. And we want to make sure we get them where they need to be and that they're going to be able to function at the level they want to. And that includes going to school, taking care of their family, being able to work, being able to travel unencumbered.
So, after you've asked some of these questions, what objective measures do you use? Does it depend on the patient? Does it depend on their disease? Or how do you think about this and what do you use?
Dr. Josh Steinberg: Sure, so assessing disease is getting easier as we have labs that are noninvasive and fairly accurate in predicting endoscopic activity. As we mentioned earlier, the key ones are C-reactive protein and fecal calprotectin. The latter, of course, offers us advantageous sensitivity over the other biomarkers, meaning we can get a more accurate read on disease activity. Now, some patients may exhibit anemia and low platelets, not mounting a reliable CRP level.
For these patients, measuring albumin levels can help provide biomarker data in determining appropriate treatment strategies. Proactively, biomarkers are helpful during routine follow-ups to catch potential issues early, regardless of symptom recording.
Dr. David Rubin: Hey Josh, let's bring this to life for our listeners. Can you describe one of your patients who recently demonstrated signs of inadequate response and needed a treatment switch? Maybe a reach, because I'm sure all your patients are in remission, but maybe you can think of one. [Laughs]
Dr. Josh Steinberg: Of course, I'd wish all my patients were in remission, but as you know, we're dealing with a really complicated disease with ulcerative colitis. And many of my patients will respond, but many will lose response. So, of several examples I can think of, one was a young person who had done relatively well on an anti-TNF treatment. He responded initially and he did have a loss of response. He had worsening rectal bleeding, stool frequency, clearly elevated inflammatory markers and the stool with his calprotectin. And we knew we needed to make a switch because even though this patient had an initial response, clearly, they had a secondary loss of response to this treatment.
Dr. David Rubin: Josh, once it's been determined that a patient might benefit from switching to another therapy, how do you actually have that conversation? Because a lot of times what happens is a patient is finally trying a new therapy or has been on a therapy that was working and there's a lot of inertia to move to a new treatment or to a different treatment as well as all the fear and uncertainty of whether it's gonna work. So, tell me a little bit about how you approach those patients and how you discuss making a treatment switch.
Dr. Josh Steinberg: So, it's an important question. And this whole concept of shared decision-making with our patients is really critical. And you have to really get to the patient's level. And patients might differ in terms of their understanding of their disease and of their understanding of the disease treatment options. Cause as we know, there's many options available more so than there were five years ago, let alone 10 or 20 years ago. So, we want to use our patient's understanding to really help make that decision together. And listen, I'm sensitive to a patient's kind of thought or notion that they're doing better, right? But what does better really mean, right? Are they able to go out and see their friends and family and do all the things they want to be doing? You know, is their new normal having eight to 10 bowel movements a day as opposed to 15 to 20, which sure by the numbers might be an improvement, but we know we can do better.
Dr. David Rubin: I think that's a really good approach. One of the things that I say to patients as well is I remind them that chronic inflammation in their body can affect their health in general. So, getting by with active symptoms because the patient's been able to manage their job or their workplace or be closer to a bathroom is not necessarily something that is okay in many other ways that they need to be aware about.
I also agree completely that we have to work with the patient to make these decisions so that we're all on the same page. And sometimes it takes multiple attempts. A patient may want to try the therapy they're on a little bit longer. They wanna just give it a chance. And I think that that's okay as long as we define what that means and when it's going to occur. In other words, we don't want patients to continue trying something that's clearly not working.
On the other hand, we want them to feel comfortable enough that they did do what they wanted to try, at least for a bit, before we move on to something else. And that's the give and take of being a clinician and having these conversations. Earlier today, I had a conversation with a patient who happened to be on an anti-TNF therapy that had worked for a long time, and now it's not working. And he's about to get on an airplane and travel across the country for a business trip and wanted to know what he should do now and what he should do when he gets home to try and get it under control.
And he was obviously reluctant to make a big switch in his therapy because he had such great success for so long with his current treatment. And we went through all the different possibilities and options and he's gonna be thinking about those. And when he gets back, we'll see how he's feeling, and I think he'll be more likely to move forward. I think that having a patient with active disease is an easier conversation than when we find somebody who feels improved or even well, but we see inflammation that wasn't expected.
Dr. Josh Steinberg: I agree with you. I try to really lean into that whole component of clinical remission and endoscopic remission because if we're not able to achieve those targets, we know what patients won't do as well long-term. So, you know, often I tell patients perfect can be the enemy of good, but in these circumstances, we know that we can truly do better. So, although I'm sensitive to, you know, a patient's own particular interests and maintaining their particular treatment that they're on, I want them to know that we have options that they can do better on potentially.
Dr. David Rubin: Yeah, I think that that's a really important point. And I'll also really emphasize the importance to know that we're gonna take this one step at a time, right? And that if this therapy doesn't do what we need, we're gonna try something else. But explaining to the patient the real cost of living with active inflammation.
And sometimes it's more than they even are acknowledging, not just in what they're willing to say, but in terms of how much they've normalized the way they're living or they've adjusted their lifestyle to accomplish what they need to accomplish or try to accomplish living with active ulcerative colitis. And until they get to this point where they realize what remission is supposed to be and how they should feel, they often are not aware that they could actually have a much better existence if they make the right treatment switch. And so, I do think that these conversations are difficult.
And it's often a very challenging time for us to move a patient through to a new treatment. But we also need to remember that this can happen over multiple conversations or multiple clinic visits and that we can do this with baby steps. What I say is let's try the therapy and see if it even works before we get too far down the road about discussing how long you're gonna stay on it. And I think that that's all part of helping somebody feel comfortable and confident in what we're doing.
And the last thing I'll say, and what I've taught the fellows, and I often remind my colleagues, is that when a patient isn't willing to do something that you're recommending, I think it's completely appropriate to suggest they get another opinion. And I think that that is a very helpful way either to reinforce what you're already saying or to provide the patient with the humility that they might hear from another expert and then feel more comfortable with what you've been recommending. So, I do think that that's another approach to some of these challenging interactions.
Ultimately though, when they feel better and they're in stable remission, the risk to benefit ratio in terms of their tolerance for the therapy completely changes. It's a completely new conversation after they're actually feeling better.
Dr. Josh Steinberg: I agree with you and many patients will tell me, you know, whether it's three months, six months after starting a new treatment that they wish they kind of made that decision earlier to make that change because they felt so comfortable feeling better, right? But not well, that it was hard for them to make that decision. So, once they finally get over that hump and hopefully are doing better on a newer therapy, patients are super grateful and doing incomparably better. And it makes us as physicians feel wonderful that we're able to get them to that point.
Dr. David Rubin: I say to patients that it's my job to help evaluate their condition and to make recommendations and to educate them and then ultimately to respect their decisions. And I work with them to try to get to these points.
Dr. David Rubin: So, Josh, stemming from this larger conversation about treatment switches, we’re going to talk next about a treatment option that may help our patients with moderate to severe UC who have failed or who have an intolerance to an anti-TNF. Patients should be educated on the importance of controlling their disease progression, and the risks and benefits of this therapy, which is, upadacitinib, or RINVOQ.
Clinical trials for this treatment have proved that patients can achieve durable remission with RINVOQ. Following Important Safety Information about RINVOQ, we’ll look at its comprehensive data and share our personal experience prescribing it to our anti-TNF patients who’ve had an inadequate response.
RINVOQ is a once-daily oral Janus kinase inhibitor indicated for the treatment of adults with moderately to severely active ulcerative colitis who have had an inadequate response or intolerance to one or more tumor necrosis factor blockers.
RINVOQ is not recommended for use in combination with other JAK inhibitors, biological therapies for ulcerative colitis, or with other potent immunosuppressants.
RINVOQ is contraindicated in patients with hypersensitivity to RINVOQ or its excipients.
Patients treated with RINVOQ are at an increased risk of serious infections that can lead to hospitalization or death. Most of these infections occurred in patients who were concurrently taking immunosuppressants or steroids.
A number of safety findings were observed in a study comparing another JAK inhibitor against TNF blockers in rheumatoid arthritis patients. These were patients who were 50 years and older and had one or more cardiovascular risk factors. A higher rate of all-cause mortality, thrombosis, lymphomas, and lung cancer was observed with the other JAK inhibitor. Furthermore, the JAK-inhibitor group demonstrated a higher rate of cardiovascular death, myocardial infarction, and stroke. There is increased risk for patients with a history of smoking.
Malignancies have also been reported in patients treated with RINVOQ. Patients treated with JAK inhibitors for inflammatory conditions have also experienced deep venous thrombosis, pulmonary embolism, and arterial thrombosis.
Other serious adverse reactions associated with RINVOQ include hypersensitivity reactions, gastrointestinal perforations, laboratory abnormalities, and embryo-fetal toxicity.
Please continue listening and stay tuned for additional Important Safety Information within this podcast.
Dr. David Rubin: RINVOQ had two 8-week multi-center double-blind placebo-controlled induction trials in ulcerative colitis and met its primary endpoint of clinical remission. Participants on RINVOQ who achieved clinical response at Week 8 with 45 mg of RINVOQ were moved into the U-ACHIEVE maintenance trial. The clinical trials had a primary endpoint of clinical remission, which was defined as no rectal bleeding, reduced stool frequency, and an endoscopic subscore of less than or equal to 1 without friability.
It also had ranked secondary endpoints, which included clinical response per the adapted Mayo score, endoscopic improvement, and histo-endoscopic mucosal improvement. All primary and secondary endpoints were achieved.
In clinical trials, RINVOQ provided rapid relief of rectal bleeding and stool frequency as early as Week 2. The ranked secondary endpoint of clinical response per partial modified Mayo score is a composite of the Mayo stool frequency and rectal bleeding subscores and is defined as a decrease in total score more than or equal to 30% and more than or equal to one point from baseline and a decrease in rectal bleeding subscore more than or equal to 1 or a rectal bleeding subscore of 0 or 1.
In the U-ACHIEVE induction trial at Week 2, 60% of the 319 patients on RINVOQ 45 milligrams achieved clinical response compared to only 27% of the 154 patients on placebo, measured by a decrease in rectal bleeding and stool frequency. Pretty remarkable.
Dr. Josh Steinberg: I agree. And so, what I see within that data is that it addresses the fact that patients want to feel better quickly.
Dr. David Rubin: What I say to patients when I start this therapy is that they should expect to feel well quickly in most cases, and this is something that they can expect to notice within the first couple weeks.
Dr. Josh Steinberg: Yeah, after response, however, both patients and clinicians are looking for and value a durable remission.
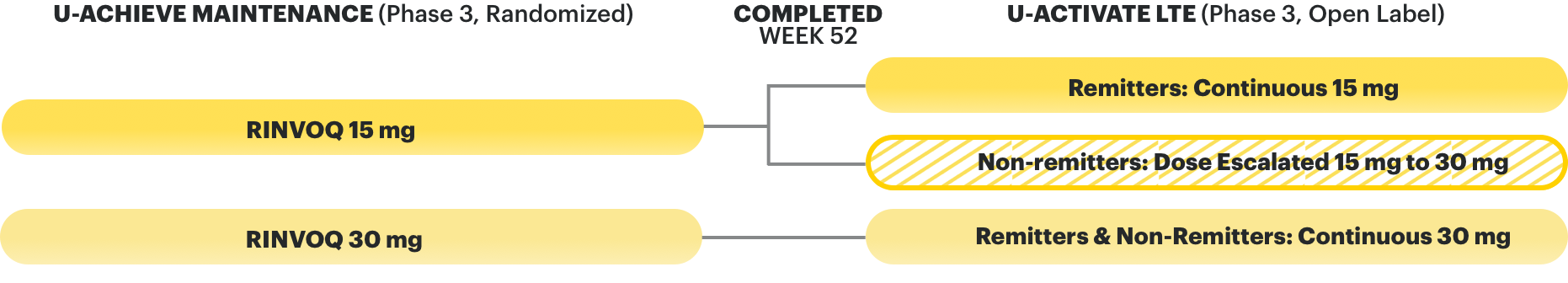
Dr. David Rubin: So that's what we'll discuss next. Following the 8-week induction trials, the subsequent 52-week U-ACHIEVE maintenance trial randomized the induction responders to receive either placebo, RINVOQ 15 milligrams or RINVOQ 30 milligrams once daily.
In the 52-week maintenance trial, RINVOQ met its primary endpoint, demonstrating durable remission at Week 52. 42% of the 148 patients on RINVOQ 15 milligrams and 52% of the 154 patients on RINVOQ 30 milligrams achieved clinical remission, compared to 12% of the 149 patients on placebo. A dose of 30 milligrams once daily may be considered for patients with refractory, severe, or extensive disease. And you should discontinue RINVOQ if an adequate therapeutic response is not achieved with the 30 mg dose.
Data are also available for RINVOQ's open-label extension, the U-ACTIVATE study. In an open-label extension, there is a potential for enrichment of the long-term data in the remaining patient populations, since patients who are unable to tolerate or who do not respond to the drug often drop out. In an as-observed analysis, missing visit data were excluded from calculations for that visit, which may increase the percentage of responders. All observed data was used regardless of premature discontinuation of study drug or initiation of concomitant medications. The same patient may not have a response at each time point. All patients who completed the maintenance trial were eligible for the open-label extension trial. The RINVOQ 15-milligram arm includes patients who were in remission at the completion of the U-ACHIEVE maintenance trial and taking continuous RINVOQ 15 milligrams.
The 30-milligram arm includes both patients who were in remission and patients who were not in remission from the maintenance trial regardless of remission status. The interim analysis includes 87 patients on continuous RINVOQ 15 milligrams and 151 patients on RINVOQ continuous 30 milligrams following the U-ACHIEVE maintenance trial.
Dr. David Rubin: At Week 100, 78% of 87 patients on continuous RINVOQ 15 milligrams and 69% of 151 patients on continuous RINVOQ 30 milligrams achieved clinical remission on RINVOQ. The difference in remission status upon entrance to the U-ACTIVATE open-label extension may explain the difference in efficacy between the 15- and 30-milligram arms.
Narrator: Week 100 mentioned previously is intended to mean Week 48 of open-label extension, OLE, and Week 100 overall.
Dr. David Rubin: So, I think it was helpful to review the clinical trial data, but let’s hear from you about how it matches your clinical experience. And I'll tell you that in my clinical experience, I've had similar results and we've been really pleased with seeing how this can be an effective option for our patients with moderate to severe UC.
Dr. David Rubin: So, Josh, I know you've prescribed RINVOQ for some of your patients. Do you think that your results match what we saw in the clinical trials?
Dr. Josh Steinberg: David, I have to say I'm quite impressed with RINVOQ’s clinical trial results, not just in terms of the clinical remission data, but especially the endoscopic response and remission data too. And again, we're talking about an oral small molecule, a once-daily pill, that really has the potential to help some of our patients who have been refractory or intolerant to anti-TNF agents and get them feeling better. And we know per the data and the clinical trials that they can get feeling better quite soon, right? Within two weeks. And that really does match my personal experience. We often talk about this concept of a steroid-free remission and staying off steroids long term is of utmost importance for us and for our patients. And in the RINVOQ clinical trials, which did look at steroid-free remission as a ranked secondary endpoint, this endpoint was achieved. So, I'm quite pleased with the clinical trial. And again, in my personal clinical experience and I know amongst the clinical experience of my colleagues, I would say that largely my personal experience does match the clinical trial results.
So, I've had patients start on RINVOQ with a broad spectrum of disease activity. So, in patients with more severe disease, those patients who were on anti-TNF agents, that we couldn't get them into a durable remission. And I've also had more moderate activity patients that I've started on RINVOQ who were refractory and intolerant to our anti-TNFs. And in general, I've had success with my patients who I started on RINVOQ in both the short and long term, now that I've been using it for the last year and a half or so since it was initially approved.
Dr. David Rubin: You know, I think it's really important to recognize that it has steroid-sparing effects and met that secondary endpoint, but I also want to remind everyone that 60% or more of the patients that were in the clinical trials were not even on steroids on entry. So, we can also avoid steroids completely, which is something I think we should be doing more of, especially if we can get them on therapy quickly.
Dr. David Rubin: So, Josh, previously you shared a story about one of your patients who had an inadequate response to their anti-TNF. Can you tell us a little bit more about what your treatment decision was in that situation and the outcome of the switch?
Dr. Josh Steinberg: Definitely. So, I encountered a patient with UC who faced breakthrough symptoms despite being on an anti-TNF agent. And the patient's treatment history comprised of various mesalamine formulations orally and rectally, corticosteroids, immunomodulators. But unfortunately, their symptoms did persist, causing significant distress for the patient and their family. These symptoms included frequent bloody diarrhea, abdominal pain, weight loss, leading to a notable decline in their overall well-being.
So, recognizing these challenges posed by the inadequate response to an anti-TNF therapy, we did explore alternative options. And following a comprehensive discussion, we decided to transition the patient to RINVOQ, given its potential efficacy in cases where anti-TNFs were ineffective. The patient was successfully able to achieve clinical remission without the need for steroids using RINVOQ.
And I recently scoped the patient and I was so pleased to see that he did have endoscopic improvement.
Dr. David Rubin: Why did you think RINVOQ was the right option for your patient?
Dr. Josh Steinberg: So, based on the data from RINVOQ and my personal experience, I knew it was a great option and valued the rapid relief and durable remission.
Dr. David Rubin: So, in your practice, who do you think is the appropriate patient to receive RINVOQ, and who would not be appropriate to receive RINVOQ?
Dr. Josh Steinberg: For all medications, it's important to weigh the benefits and the risks for the individual patient when making a treatment decision. I also consider the risk of uncontrolled disease. And once I've identified a potential patient for RINVOQ, I confirm that the patient has had an inadequate response to an anti-TNF agent, and I perform tuberculosis tests, blood work including a CBC, hepatitis screen, hepatic function, and I confirm a negative pregnancy status before starting treatment. Patients who experience a prior anti-TNF failure further back in their treatment history are also candidates and important to keep in mind. We don't want to dismiss a potentially therapeutic treatment just because someone isn't actively failing or not tolerating an anti-TNF, especially if they're having a poor experience with their current therapy.
So, I consider cardiovascular and venous thromboembolism risk factors. Patients over 65 with a history of a cardiac event will give increased concern, so it is crucial to conduct risk stratification of patients before initiating treatment. While having a cardiovascular condition is not considered a contraindication, it is essential to carefully evaluate the risks and benefits specific to each individual patient.
Being a woman of childbearing age is not a contraindication for RINVOQ and may be an appropriate treatment option if it was deemed so. However, I don't consider RINVOQ for women who are pregnant or actively planning for a pregnancy.
For more information on the safety profile of RINVOQ including long-term safety data, I encourage you to visit the RINVOQ website for Healthcare Providers or contact your local representative.
Dr. David Rubin: So, I think, Josh, that you've outlined some very important points. First of all, the choice of the right patient for this therapy and who we should be thinking about. And in general, I think this is an excellent option for our patients with moderate to severe UC after they've been exposed to an anti-TNF if it's not working and they're not tolerating that therapy. I would also add that I wouldn't use it in a woman who was pregnant, but I would certainly treat a woman who was of childbearing age, and I think that that's completely appropriate and reasonable.
Dr. David Rubin: I want to thank Dr. Josh Steinberg for taking the time today to assess when there is an inadequate response and evaluate the need to transition treatments for patients with moderate to severe UC, how to include the patient in the conversation, and discussing RINVOQ as a treatment option. I look forward to seeing treatment options for patients with moderate to severe UC continue to expand and certainly to help our colleagues understand when they should use them.
Dr. Josh Steinberg: David, thank you so much. This was an absolute pleasure. And I really hope that we hear more from you and from your future guests in the Gut Reactions podcast.
Narrator
IMPORTANT SAFETY INFORMATION
SERIOUS INFECTIONS
Patients treated with RINVOQ are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants, such as methotrexate or corticosteroids. If a serious infection develops, interrupt RINVOQ until the infection is controlled.
Reported infections include:
- Active tuberculosis (TB), which may present with pulmonary or extrapulmonary disease. Test patients for latent TB before RINVOQ use and during therapy. Consider treatment for latent TB infection prior to RINVOQ use.
- Invasive fungal infections, including cryptococcosis and pneumocystosis.
- Bacterial, viral, including herpes zoster, and other infections due to opportunistic pathogens.
Carefully consider the risks and benefits of treatment with RINVOQ prior to initiating therapy in patients with chronic or recurrent infection. Monitor patients closely for the development of signs and symptoms of infection during and after treatment with RINVOQ, including the possible development of TB in patients who tested negative for latent TB infection prior to initiating therapy.
MORTALITY
In a large, randomized, postmarketing safety study comparing another Janus kinase (JAK) inhibitor with tumor necrosis factor (TNF) blockers in rheumatoid arthritis (RA) patients greater than or equal to 50 years old with at least one cardiovascular (CV) risk factor, a higher rate of all-cause mortality, including sudden CV death, was observed with the JAK inhibitor. Consider the benefits and risks for the individual patient prior to initiating or continuing therapy with RINVOQ.
MALIGNANCIES
Lymphoma and other malignancies have been observed in patients treated with RINVOQ.
In a large, randomized, postmarketing safety study comparing another JAK inhibitor with TNF blockers in RA patients, a higher rate of malignancies (excluding non-melanoma skin cancer [NMSC]), lymphomas, and lung cancer (in current or past smokers) was observed with the JAK inhibitor. Patients who are current or past smokers are at additional increased risk.
With RINVOQ, consider the benefits and risks for the individual patient prior to initiating or continuing therapy, particularly in patients with a known malignancy (other than a successfully treated NMSC), patients who develop a malignancy when on treatment, and patients who are current or past smokers. NMSCs have been reported in patients treated with RINVOQ. Periodic skin examination is recommended for patients who are at increased risk for skin cancer. Advise patients to limit sunlight exposure by wearing protective clothing and using sunscreen.
MAJOR ADVERSE CARDIOVASCULAR EVENTS
In a large, randomized, postmarketing study comparing another JAK inhibitor with TNF blockers in RA patients greater than or equal to 50 years old with at least one CV risk factor, a higher rate of major adverse cardiovascular events (defined as cardiovascular death, myocardial infarction, and stroke) was observed with the JAK inhibitor. Patients who are current or past smokers are at additional increased risk. Discontinue RINVOQ in patients that have experienced a myocardial infarction or stroke.
Consider the benefits and risks for the individual patient prior to initiating or continuing therapy with RINVOQ, particularly in patients who are current or past smokers and patients with other CV risk factors. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
THROMBOSIS
Thrombosis, including deep venous thrombosis, pulmonary embolism, and arterial thrombosis have occurred in patients treated with JAK inhibitors used to treat inflammatory conditions. Many of these adverse events were serious and some resulted in death.
In a large, randomized, postmarketing study comparing another JAK inhibitor to TNF blockers in RA patients greater than or equal to 50 years old with at least one CV risk factor, a higher rate of thrombosis was observed with the JAK inhibitor. Avoid RINVOQ in patients at risk. Patients with symptoms of thrombosis should discontinue RINVOQ and be promptly evaluated.
HYPERSENSITIVITY
RINVOQ is contraindicated in patients with known hypersensitivity to upadacitinib or any of its excipients. Serious hypersensitivity reactions, such as anaphylaxis and angioedema, were reported in patients receiving RINVOQ in clinical trials. If a clinically significant hypersensitivity reaction occurs, discontinue RINVOQ and institute appropriate therapy.
GASTROINTESTINAL PERFORATIONS
Gastrointestinal (GI) perforations have been reported in clinical trials with RINVOQ. Monitor RINVOQ-treated patients who may be at risk for gastrointestinal perforation (e.g., patients with a history of diverticulitis and patients taking NSAIDs or corticosteroids). Promptly evaluate patients presenting with new onset abdominal pain for early identification of GI perforation.
LABORATORY ABNORMALITIES
Neutropenia
Treatment with RINVOQ was associated with an increased incidence of neutropenia (absolute neutrophil count [ANC] less than 1000 cells per millimeter cubed). Treatment with RINVOQ is not recommended in patients with an ANC less than 1000 cells per millimeter cubed. Evaluate neutrophil counts at baseline and thereafter according to routine patient management.
Lymphopenia
Absolute lymphocyte counts (ALC) less than 500 cells per millimeter cubed were reported in RINVOQ-treated patients. Treatment with RINVOQ is not recommended in patients with an ALC less than 500 cells per millimeter cubed. Evaluate at baseline and thereafter according to routine patient management.
Anemia
Decreases in hemoglobin levels to less than 8 grams per deciliter were reported in RINVOQ-treated patients. Treatment should not be initiated or should be interrupted in patients with hemoglobin levels less than 8 grams per deciliter. Evaluate at baseline and thereafter according to routine patient management.
Lipids
Treatment with RINVOQ was associated with increases in lipid parameters, including total cholesterol, low-density lipoprotein cholesterol, and high-density lipoprotein cholesterol. Manage patients according to clinical guidelines for the management of hyperlipidemia. Evaluate patients 12 weeks after initiation of treatment and thereafter according to the clinical guidelines for hyperlipidemia.
Liver enzyme elevations
Treatment with RINVOQ was associated with increased incidence of liver enzyme elevation compared to placebo. Evaluate at baseline and thereafter according to routine patient management. Prompt investigation of the cause of liver enzyme elevation is recommended to identify potential cases of drug-induced liver injury. If increases in aspartate aminotransferase or alanine aminotransferase are observed during routine patient management and drug-induced liver injury is suspected, RINVOQ should be interrupted until this diagnosis is excluded.
EMBRYO-FETAL TOXICITY
Based on findings in animal studies, RINVOQ may cause fetal harm when administered to a pregnant woman. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with RINVOQ and for 4 weeks after the final dose. Verify pregnancy status of females of reproductive potential prior to starting treatment with RINVOQ.
VACCINATION
Avoid use of live vaccines during, or immediately prior to, RINVOQ therapy. Prior to initiating RINVOQ, patients should be brought up to date on all immunizations, including prophylactic varicella zoster or herpes zoster vaccinations, in agreement with current immunization guidelines.
MEDICATION RESIDUE IN STOOL
Reports of medication residue in stool or ostomy output have occurred in patients taking RINVOQ. Most reports described anatomic or functional GI conditions with shortened GI transit times. Instruct patients to contact their healthcare provider if medication residue is observed repeatedly. Monitor patients clinically and consider alternative treatment if there is an inadequate therapeutic response.
LACTATION
There are no data on the presence of RINVOQ in human milk, the effects on the breastfed infant, or the effects on milk production. Available data in animals have shown the excretion of RINVOQ in milk. Advise patients that breastfeeding is not recommended during treatment with RINVOQ and for 6 days after the last dose.
HEPATIC IMPAIRMENT
RINVOQ is not recommended for use in patients with severe hepatic impairment.
ADVERSE REACTIONS
The most common adverse reactions in RINVOQ clinical trials were upper respiratory tract infections, herpes zoster, herpes simplex, bronchitis, nausea, cough, pyrexia, acne, headache, increased blood creatine phosphokinase, hypersensitivity, folliculitis, abdominal pain, increased weight, influenza, fatigue, neutropenia, myalgia, influenza-like illness, elevated liver enzymes, rash, and anemia.
Inform patients that retinal detachment has been reported in clinical trials with RINVOQ. Advise patients to immediately inform their healthcare provider if they develop any sudden changes in vision while receiving RINVOQ.
Dosage Forms and Strengths: RINVOQ is available in 15 mg, 30 mg, and 45 mg extended-release tablets.